Differences in dose-response relationships among commonly used antidepressants
Many commonly used SSRIs and SNRIs exhibit optimal therapeutic effect treating major depressive disorder (MDD) when ~80% of the serotonin transporter (SERT) is inhibited or occupied.†1 As such, the approved dose ranges are at this level of SERT occupancy.1
If patients with MDD do not respond adequately to their antidepressant treatment, what therapeutic effect can be expected by increasing the dose of SNRIs and SSRIs?
A meta-analysis was conducted to assess the dose response relationships of five different SSRIs in acute treatment of adults with MDD. Doses of citalopram, escitalopram, paroxetine and sertraline were converted to fluoxetine equivalents to allow comparison between dosage regimes.2 Results indicated that for each SSRI studied, the dose response curve showed a gradual increase up to doses between 20 mg and 40 mg fluoxetine equivalents, and a flat to decreasing trend through the higher licensed doses up to 80 mg fluoxetine equivalents, as the SERT occupancy achieved a plateau at higher doses.2
However, increasing doses of SSRIs were associated with a linear to exponential increase in the rate of dropouts due to adverse events (AEs) at the upper limit of the approved dose range of fluoxetine equivalents.2
Increasing doses of SSRIs were not associated with increasing response rates, but were associated with an increase in AEs‡2
Meta-analysis: Dose-response relationships for SSRIs
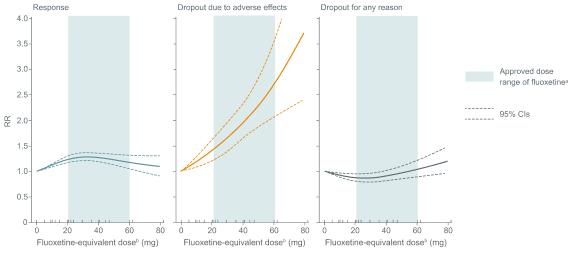
Adapted from Furukawa TA et al. 2019. Each tick on the x-axis represents the dose examined in a treatment group. RR, risk ratio.
a Obtained from the Summary of Product Characteristics for fluoxetine.
b Doses of citalopram, escitalopram, paroxetine and sertraline were converted to fluoxetine equivalents
Such increasing rates of AEs may lead to treatment discontinuation3,4, which could result in an increased risk of relapse or reduced quality of life.4
Adapted from Furukawa TA et al. 2019. Each tick on the x-axis represents the dose examined in a treatment group. RR, risk ratio.
a Obtained from the Summary of Product Characteristics for fluoxetine.
b Doses of citalopram, escitalopram, paroxetine and sertraline were converted to fluoxetine equivalents
Such increasing rates of AEs may lead to treatment discontinuation3,4, which could result in an increased risk of relapse or reduced quality of life.4
Watch the video of Professor Andrea Fagiolini, discuss the considerations when determining the optimal dose of antidepressants, taking into account the relationship between dose and efficacy and between dose and adverse events of antidepressants in the treatment of MDD.
Watch the video of Professor Andrea Fagiolini, discuss the considerations when determining the optimal dose of antidepressants, taking into account the relationship between dose and efficacy and between dose and adverse events of antidepressants in the treatment of MDD.
‡ Striatal 5-HTT binding potential measured in 77 subjects before and after 4 weeks of medication administration. Binding potential is proportional to the density of receptors not blocked by medication. Subjects received citalopram, fluoxetine, sertraline, paroxetine, or extended-release venlafaxine. Healthy subjects received subtherapeutic doses; subjects with mood and anxiety disorders received therapeutic doses.1
‡ Dose response relationships for SSRIs in 99 treatment groups.2
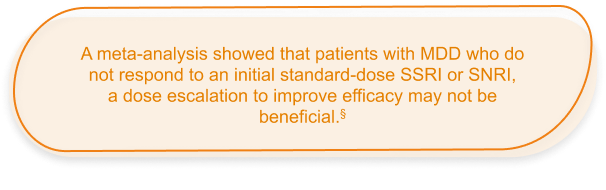
§ Data based on a meta-analysis of 7 double-blind, parallel-group studies comparing a dose increase of SSRI/SNRIs directly to continuation of standard-dose treatment in patients with MDD who did not respond to SSRI/SNRI treatment. No significant difference in mean HAM-D total score change was observed between the dose escalation group and the group who continued the initial treatment dose (Hedges g=-0.04, p=0.63).5
Abbreviations:
AE, adverse event; MDD, major depressive disorder; SERT, serotonin reuptake transporter; SNRI, serotonin and norepinephrine reuptake inhibitors; SSRI, selective serotonin reuptake inhibitors
‡ Striatal 5-HTT binding potential measured in 77 subjects before and after 4 weeks of medication administration. Binding potential is proportional to the density of receptors not blocked by medication. Subjects received citalopram, fluoxetine, sertraline, paroxetine, or extended-release venlafaxine. Healthy subjects received subtherapeutic doses; subjects with mood and anxiety disorders received therapeutic doses.1
‡ Dose response relationships for SSRIs in 99 treatment groups.2
§ Data based on a meta-analysis of 7 double-blind, parallel-group studies comparing a dose increase of SSRI/SNRIs directly to continuation of standard-dose treatment in patients with MDD who did not respond to SSRI/SNRI treatment. No significant difference in mean HAM-D total score change was observed between the dose escalation group and the group who continued the initial treatment dose (Hedges g=-0.04, p=0.63).5
Abbreviations:
AE, adverse event; MDD, major depressive disorder; SERT, serotonin reuptake transporter; SNRI, serotonin and norepinephrine reuptake inhibitors; SSRI, selective serotonin reuptake inhibitors