Why does extreme emotional trauma cause post-traumatic stress disorder (PTSD) in some people, but not others? Why do two-thirds of people with PTSD have an alcohol/substance use disorder (A/SUD)? Current knowledge about the genetics and neurobiology responsible for response to extreme emotional trauma and vulnerability to A/SUD, and the adverse impact of PTSD and A/SUD comorbidity on a variety of outcomes were highlighted by Mark Hamner and Karen Hartwell of the Medical University of South Carolina Charleston, South Carolina, at Psych Congress 2019.
Factors determining response to extreme emotional trauma
Resilience to extreme emotional trauma varies within the society, with some people being more resilient than others, explained Professor Hamner. The individual response depends on genetic predisposition, psychological coping strategies, environmental factors and epigenetic factors.
Little is known about the genetics for A/SUD
In terms of genetic predisposition, Professor Hamner described an association between the SS (short alleles) genotype of the serotonin transporter gene promoter region (5-HTTLPR) and PTSD in people exposed to high trauma.1
Little is known about the genetics for A/SUD, said Professor Hartwell, but 5-HTTLPR predicts PTSD comorbid with AUD.2
The neural circuitry of fear
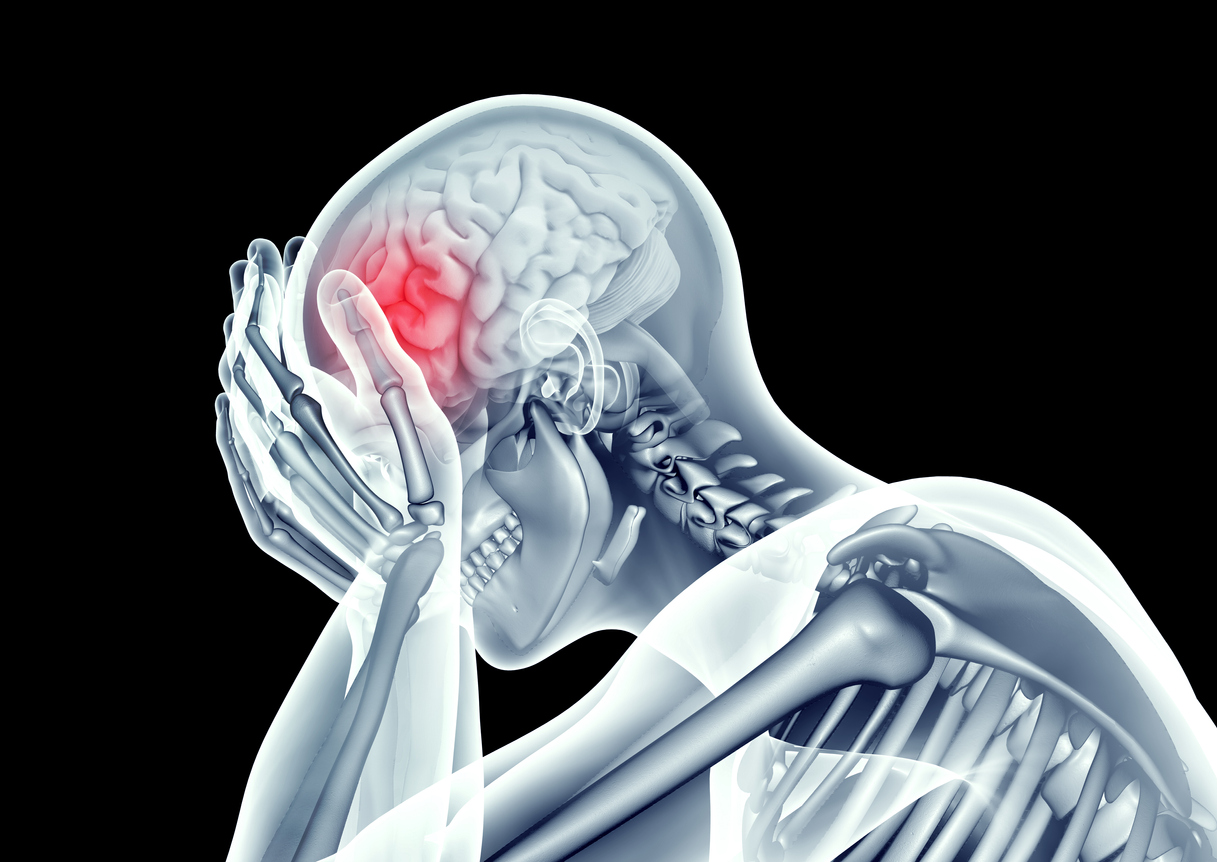
PTSD arises from dysregulation in the neural circuitry of fear, explained Professor Hamner. It is characterized by increased activation of the amygdala, which is responsible for conditioned fear and associative emotional learning. Amygdala activity is in turn regulated by:
- the hippocampus, which plays a role in explicit memories of traumatic events and in mediating learned responses to contextual cues
- the prefrontal cortex, which is responsible for reactivating past emotional associations3
PTSD is characterized by increased amygdala activation, regulated by hippocampus and prefrontal cortex
A meta-analysis of 19 functional neuroimaging studies of symptom provocation, in 274 patients with PTSD compared to controls, revealed significant activation of the mid-line retrosplenial cortex and precuneus in response to trauma-related stimuli in PTSD, said Professor Hamne. Such activation suggests enhanced self-referential processing and recreation of relevant autobiographical memory in PTSD.4
Multiple neurotransmitters and neurohormones play a role
Many neurotransmitters play a role in PTSD7 including:
- dopamine — though more research is needed to understand how it affects the development and maintenance of PTSD
- serotonin — which also plays a role in A/SUD and associated psychiatric disorders
- norepinephrine — which is increased5
- cortisol — which is decreased5
- neuropeptide Y (NPY) — which is abundant in forebrain limbic and brain stem and regulates stress and emotional behaviors — NPY concentration or function may be decreased in PTSD6
- various neurohormones7
PTSD and A/SUD often occur together
A/SUD can have a negative impact on the course of PTSD
Comorbidity of PTSD and A/SUD is extremely high, said Professor Hartwell, and associated with poorer outcomes than having either disorder alone across a variety of psychological, functional, and treatment outcomes, specifically:8
- greater psychological distress
- diminished social functioning
- poorer treatment adherence
- increased AUD-related problems8
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.