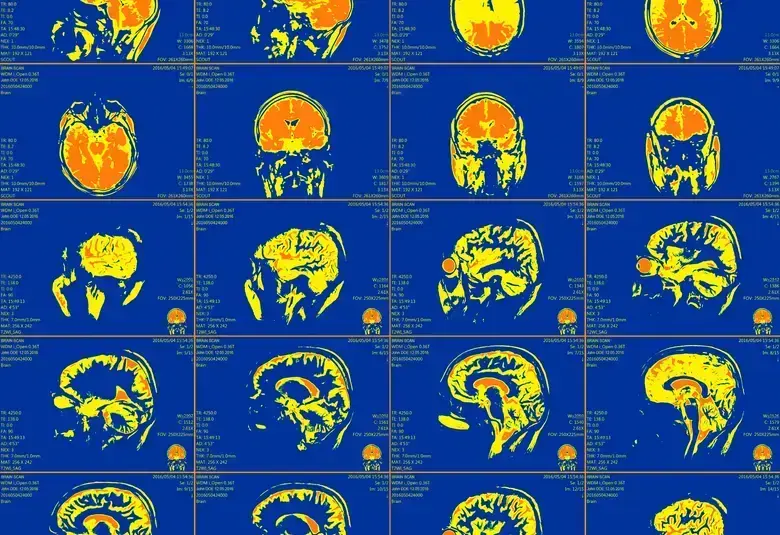
The brains of people with Alzheimer’s disease contain abnormal proteins—amyloid-beta and phosphorylated tau. Over time, amyloid-beta plaques, which are first seen in the neocortex, increase in number and involve all brain regions. Dementia occurs only when the plaques involve the midbrain and medulla oblongata. How the dementia appears clinically is then influenced by other brain abnormalities commonly seen in elderly people, explained Professor Dietmar Thal, Leuven, Belgium, in a fascinating educational session at EAN 2021.
Abnormal amyloid-beta and phosphorylated tau protein deposits
Neurofibrillary tangles and senile plaques are hallmarks of Alzheimer’s disease
Characteristic changes are seen in the brains of people with Alzheimer’s disease, explained Professor Thal. These changes are:
- Neurofibrillary tangles, which are intraneuronal aggregates of abnormal phosphorylated tau protein
- Senile plaques, which are extracellular aggregates of amyloid-beta (Aβ) protein1
The presence of Aβ protein plaques in the brain follows a distinct hierarchical sequence with gradual progression into regions that receive neuronal projections from regions already containing Aβ plaques.
Amyloid-beta deposition follows a distinct hierarchical sequence
Five phases can be identified as the plaques spread throughout the brain,2 said Professor Thal.
- In phase 1, one or more Aβ plaques are found in the frontal, occipital, parietal and/or temporal neocortex
- In phase 2, Aβ plaques are seen in the allocortex—the entorhinal cortex, the hippocampus, and the cingulate gyrus
- In phase 3, the distribution of Aβ plaques includes the thalamus, the hypothalamus, and the basal ganglia, and by this phase, the entire neocortex is filled with Aβ plaques
Only the final two phases of amyloid-beta deposition are associated with dementia
- In phase 4, Aβ plaques are present in the midbrain and in the medulla oblongata
- In phase 5, Aβ plaques are seen in the pons and cerebellum
Dementia is only seen in patients with phase 4 or 5 Aβ plaques, added Professor Thal. It is not usually seen patients with phase 1, 2, or 3 Aβ plaques.
Other brain pathologies contributing to the Alzheimer’s dementia phenotype
Alzheimer’s dementia is a heterogeneous disease
Professor Thal highlighted that the brains of many elderly people show changes not only of Alzheimer’s disease, but also many other pathologies, including:
- Cerebral amyloid angiopathy3
- Small vessel disease3
- Atherosclerosis of the circle of Willis3
- Granulovacuolar degeneration4
- Limbic-associated age-related transactive response DNA-binding protein (TDP)-43 encephalopathy (LATE)5
- Lewy body disease6
These brain pathologies can all contribute to the dementia phenotype, explained Professor Thal.
A diagnosis of dementia should include all brain pathologies
In addition, specific brain pathologies such as argyrophilic grain disease, which affects 5% of all patients with dementia, has additive effects on the cognitive symptoms associated with Alzheimer’s disease.7
A diagnosis of dementia should therefore include all pathologies, and combined treatment strategies may be more effective than a treatment strategy targeting a single pathology, concluded Professor Thal. This has implications for the design of clinical trials investigating drugs targeting Alzheimer’s disease.
For the latest updates on sea.progress.im, subscribe to our Telegram Channel https://bit.ly/telePiM
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.