Around 21% of patients with schizophrenia achieve clinical recovery – a statistic that hasn’t changed in recent years, despite advancements in psychopharmacology.1 Given this reality, there is an urgent need to identify more effective ways to deliver care to patients with psychosis, schizophrenia, and other mental illnesses. This was the focus of several sessions at EPA 2023: The 31st European Congress of Psychiatry, which took place in Paris in March 2023.
While there is no one-size-fits-all approach to treatment for mental illnesses – a topic explored in depth during the congress by Professor Nandini Chakraborty of the University of Leicester’s Department of Health Sciences and Leicestershire Partnership NHS Trust, UK – a combination of long-acting injectable (LAI) treatments and shared decision-making between patients and care teams can help clinicians co-develop more effective care plans together with their patients.
With treatment that takes into account patients’ unique needs and values, administered at a cadence that patients can stick to, clinicians can help encourage medication adherence and reduce the risk of relapse.
Latest findings related to care for patients with psychosis and schizophrenia
Given the need for more effective treatment options for patients with psychosis, Professor Chakraborty introduced recent discoveries that power new understanding of the drivers of psychosis, as well as how to treat it. She presented these studies during a session titled “Best of 2022 – What's new about psychosis”.2
One publication Professor Chakraborty presented demonstrated a new potential biomarker for vulnerability to psychotic-like experiences in adolescents, which then transitions to psychosis.3 Another publication explored the identification of genes which predict a vulnerability to schizophrenia,4 and a third provided evidence of patients’ real-world experiences with an antipsychotic medication used to treat negative symptoms of psychosis.5
Clinicians should keep up to date with the latest research to inform discussions with patients and their caregivers
Throughout the session, Professor Chakraborty emphasized the importance of clinicians keeping up to date with the latest research to inform discussions with their patients and their caregivers. She presented an example of a relatively new and trending treatment modality known as Open Dialogue, which approaches schizophrenia and psychosis as a response to relational difficulties and delivers treatment via facilitated discussions with patients and their social networks.6 While randomized controlled trials on the effectiveness of Open Dialogue are underway, the field lacks concrete data of its efficacy. Nonetheless, Open Dialogue has been featured as a front-page news story, meaning patients and caregivers may ask providers questions about it.
“Emotiveness and the involvement of family within treatments is not something that we should deny,” Professor Chakraborty said. “We have to be aware of the various perspectives around psychosis and schizophrenia.”
Open Dialogue, a relatively new and trending treatment modality, approaches schizophrenia and psychosis as a response to relational difficulties and delivers treatment via facilitated discussions
Despite new advancements in psychiatric care, Professor Chakraborty presented one study that explored the relationship between schizophrenia, comorbid substance use, and treatment in over 45,000 patients.7 The study found that the risks of developing substance use disorder and being admitted to the hospital were reduced using some current and standard treatments, antipsychotic polytherapy, and LAIs.7
At the end of her presentation, Professor Chakraborty reiterated the importance of clinicians taking a holistic approach to designing psychological treatment plans that work – and that are sustainable for patients, in order to avoid non-adherence and relapse.
Clinicians stand between all the different psychological and neuroscientific advancements and the specific needs of the patient in front of them, she explained. “We need to bring these strands together.”
How long-acting injectables support improved outcomes?
One of the most significant barriers to long-term maintenance treatment of illnesses, like psychosis or schizophrenia, is relapse. During the industry-sponsored satellite symposium* titled “Improving the treatment journey during the maintenance phase: What are the clinical considerations?” Professor Christoph Correll – Professor of Child and Adolescent Psychiatry at Charité Universitätsmedizin Berlin, Germany and Professor of Psychiatry and Molecular Medicine at The Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, USA – described relapse as the “gorilla in the room.”8
“We need to stay engaged with our patients and have them be engaged in life, because relapse erodes and interrupts the neurobiological cycle, the social fabric of patients’ lives, and their hope and self-identity,” Professor Correll said.
Studies have demonstrated that each relapse is associated with a decrease in response to treatment, an increase in treatment resistance, increased symptoms and disability, greater healthcare resource usage, and neuropathological decline.9,10
To avoid relapse, Professor Correll recommended maintenance treatment with LAIs and psychosocial care. This combination of care pathways helps to ensure patients receive holistic care that can encourage them to stay on medication and reduce chance of relapse.
LAIs are especially effective when treatment begins early in a patient’s disease as a preventative approach: “Preventive psychiatry means using an LAI before there is non-adherence, before there are emergency room visits or admissions,” Professor Correll said.
Preventive psychiatry means using a long acting injectable before there is non-adherence – Professor Christoph Correll
Compared to taking daily oral medications, patients treated with LAIs – which are administered less frequently every 2 weeks to every 6 months – have better adherence, and adherence improves as the interval between treatments increases.11 Of course, Professor Correll clarified, it’s important to monitor long-term risks and benefits when choosing treatments.
In addition to medication, Professor Correll described the pillars of psychosocial wellbeing that are important to monitor to encourage long-term maintenance of a patient’s condition:
- self-care
- social interactions
- leisure time
- engagement with education or work
Earlier and more frequent offering of LAIs is a key element of preventive psychiatry — combined with psychosocial and behavioral interventions - Professor Christoph Correll
Professor Correll concluded that earlier and more frequent offering of LAIs is a key element of preventive psychiatry — combined with psychosocial and behavioral interventions – for patients with schizophrenia to avoid treatment discontinuation, relapse, hospitalization, and mortality, and to improve functioning.
Importance of shared decision-making in long-term treatment
“Clinical decision-making is a complex and dynamic social process,” Professor Gaia Sampogna of the University of Campania “L. Vanvitelli”, Italy began during the session “Shared decision-making in patients with severe mental disorders”.12 As a result, the field of psychiatry – and medicine more broadly – is shifting its decision-making model from paternalistic approach to shared decision-making to ensure patients’ needs are met and that treatment has a chance of long-term success.
Clinical decision-making is a complex and dynamic social process,” Professor Gaia Sampogna
“We’ve started to understand that the needs of patients and families must be central to the decision-making process,” Professor Sampogna said. “They can’t just receive clinical decisions without taking an active role.”
Shared decision-making aims to facilitate patient-centered care and treatment adherence by promoting joint treatment decision-making between patients with chronic conditions and clinicians, Professor Sampogna explained.13 It can help improve relationships between clinicians and patients, and it’s gained traction at a policy level worldwide; for instance, NICE in the UK has issued formal guidance on shared decision-making.
The needs of patients and families must be central to the decision-making process – Professor Gaia Sampogna
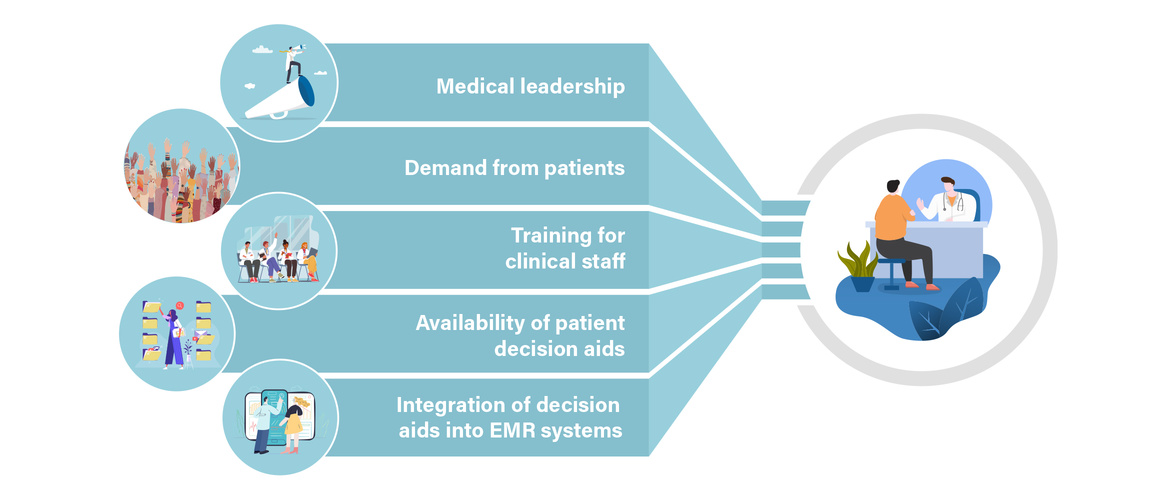
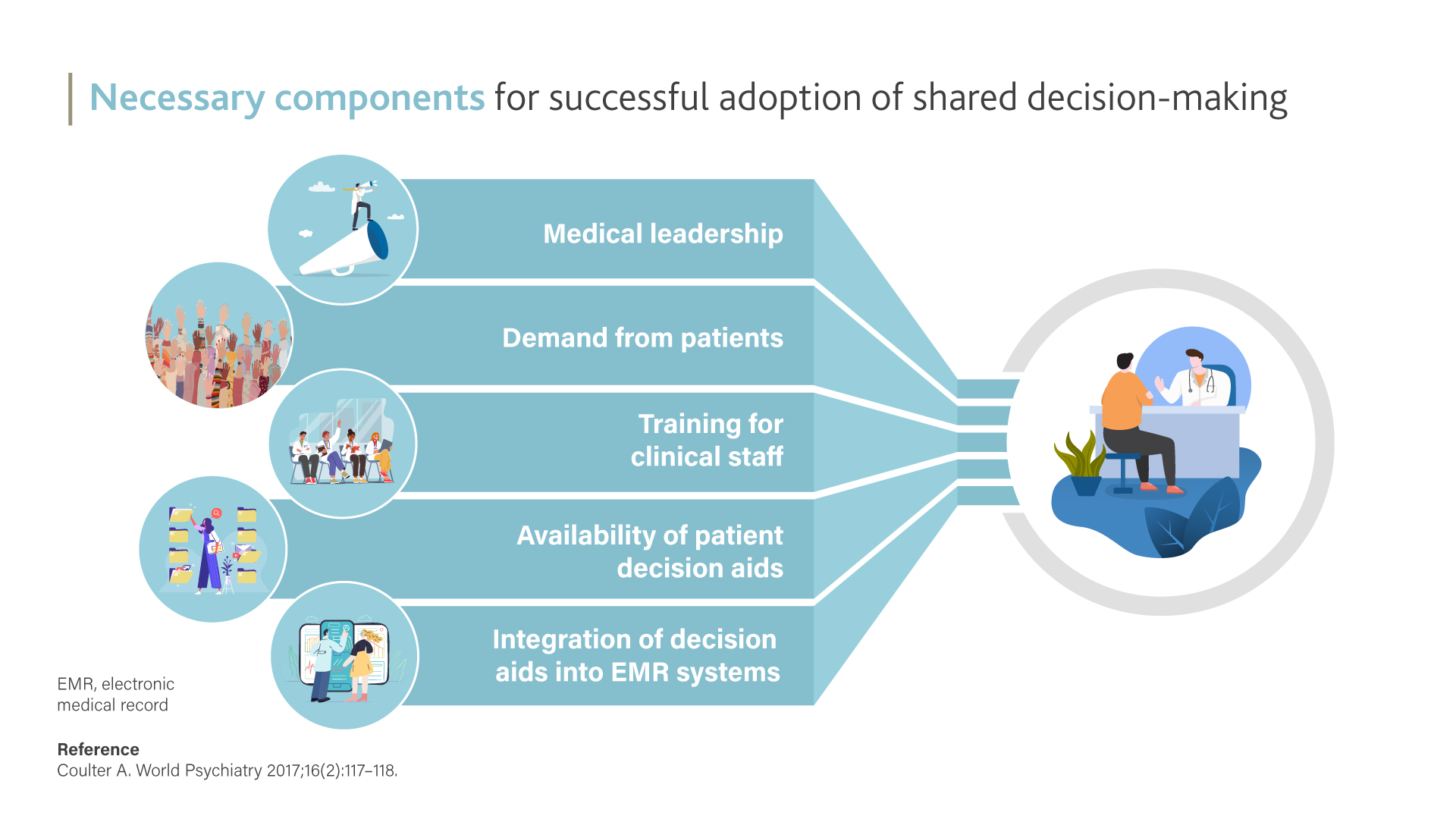
Despite its potential for facilitating improved patient care in psychology and beyond, adoption of shared decision-making has been slow. Professor Sampogna cited several necessary components to adoption, including medical leadership, demand from patients, training for clinical staff, availability of patient decision aids, and integration of decision aids into electronic medical record systems.14
To support adoption of shared decision-making in mental healthcare, a number of randomized controlled trials are underway to investigate its effectiveness. Professor Sampogna referenced the CEDAR Project, which demonstrated patients’ and providers’ preference for shared decision-making over other clinical decision-making styles.15
Enabling long-term maintenance of psychiatric conditions
While there’s still much to be done to improve outcomes and care for patients with psychosis or schizophrenia, interventions discussed during this year’s EPA congress represent a path forward.
An earlier and wider use of LAIs can help us improve outcomes – Professor Christoph Correll
“Long-term outcomes in schizophrenia remain suboptimal in many, many cases. Monitoring is a major threat and relapse is our and our patients’ main enemy,” Professor Correll said during his session. "Maintenance treatment is key to stabilizing patients to achieve better outcomes, including recovery, and an earlier use and wider use of LAIs, in our opinion, can help us improve outcomes. Clearly that needs to be also matched with psychosocial interventions to get to recovery.”
*Educational financial support for this satellite symposium was provided by Janssen Pharmaceutical Companies of Johnson & Johnson.