New EPA guidelines on the diagnosis and management of negative symptoms should help draw attention to this debilitating and sometimes overlooked aspect of schizophrenia. Their importance in the context of first episode psychosis was discussed at EPA2020 by Merete Nordentoft (University of Copenhagen, Denmark).
Negative symptoms are less visible, and hard to explain to relatives
Among the new EPA guidelines, the following recommendations are regarded as justified by Grade B level evidence:
- The “second generation” Brief Negative Symptom Scale (BNSS) and the Clinical Assessment Interview for Negative Symptoms (CAINS) can be recommended for the assessment of negative symptoms in clinical contexts. Their psychometric properties are good, and all negative symptom domains are covered. [For further reading, click here]
- Social skills training should be offered. And cognitive remediation can be considered for patients who also show cognitive symptoms.
- Exercise can be considered as part of an integrated treatment plan aimed at improving physical health.
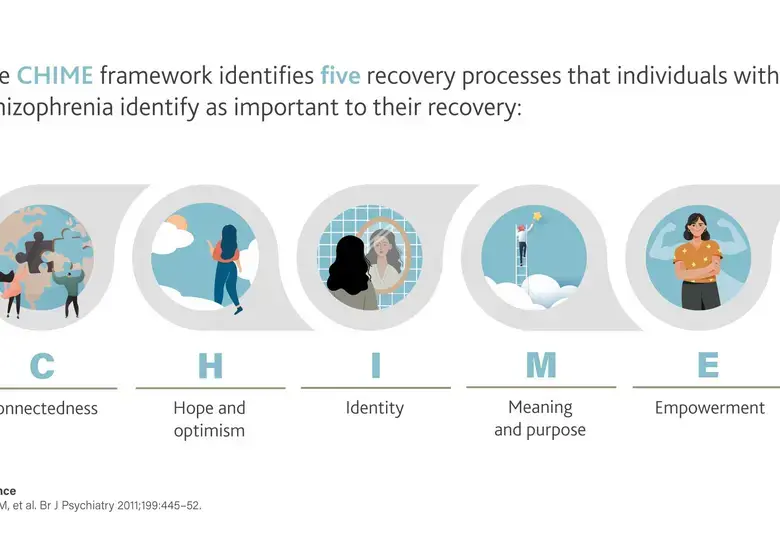
Five domains of disability
It is possible to treat negative symptoms effectively
Blunted affect, alogia, avolition, asociality and anhedonia are the principle negative symptoms, and they are present and clinically relevant in up to 60% of patients with schizophrenia.1 Interestingly, men are more severely affected by negative symptoms than women.2
The EPA guidelines acknowledge evidence that early intervention services can improve negative symptoms, and Professor Nordentoft focused on this important aspect of treatment.
According to the recent Correll et al meta-analysis of ten randomized trials, early intervention – when compared against treatment-as-usual -- significantly reduced the severity of negative symptoms, along with the severity of positive symptoms, while also improving functional outcome.3
Negative symptoms are invisible, hard to explain to family members, and can be misinterpreted as laziness or lack of willingness, Professor Nordentoft told the EPA Symposium. They are generally less well controlled by existing therapies than positive symptoms: in a cohort of 496 patients with first episode psychosis, 47% experienced a response in terms of positive symptoms, but negative symptoms responded in only 28%.4
Moreover, the persistence of negative symptoms seems to play a major role in reducing a person’s chances of being in employment, for instance.
Intervention must be extended to sustain benefit
Among other studies, the Danish OPUS program shows the value of assertive community treatment – including psycho-education and social skills training – in patients with first episode psychosis.5 At the end of the two-year period of intensive intervention, there had been a positive impact on negative symptoms.
Unfortunately, these beneficial effects diminished with time and were not evident at five or ten years, although there continued to be a positive difference compared with the treatment-as-usual controls in need for supported housing.6 The general tailing off of benefit emphasizes the need for intensive support of first-episode patients to extend beyond two years.
For the latest updates on sea.progress.im, subscribe to our Telegram Channel https://bit.ly/telePiM
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.