Making the diagnosis of a headache requires the characteristics of the headache, location, onset, severity, and so on combined with a systemic and neurological examination.
However, gathering adequate headache information for diagnosis and processing depends on several factors: the patient's ability to provide and recall essential headache information, and healthcare providers themselves should have the time and skill to draw information from patients. Nevertheless, in real practice, these factors are always incomplete.
Encouraging patients to record or make notes on a headache calendar would be one way to assist in decreasing missing data and may help in making a diagnosis.
Using the record on a headache diary or calendar, the patient and physician can also work together to find trigger headache factors, adjusting treatment based on an individual basis and the patient's responsiveness to the treatment.
Primary headaches, which have no visible intracranial pathology, are much more common than secondary headaches. Atypical headache pattern: if there is a red flag from headache history or physical examination, first consider secondary headaches that need further investigation.
Tension headaches, migraines, and cluster headaches are the three primary types of headaches. Cluster headaches are the least common of these primary headaches.
The problem is that migraines are often misdiagnosed as tension headaches.
Following IHS ICHD-3 criteria1
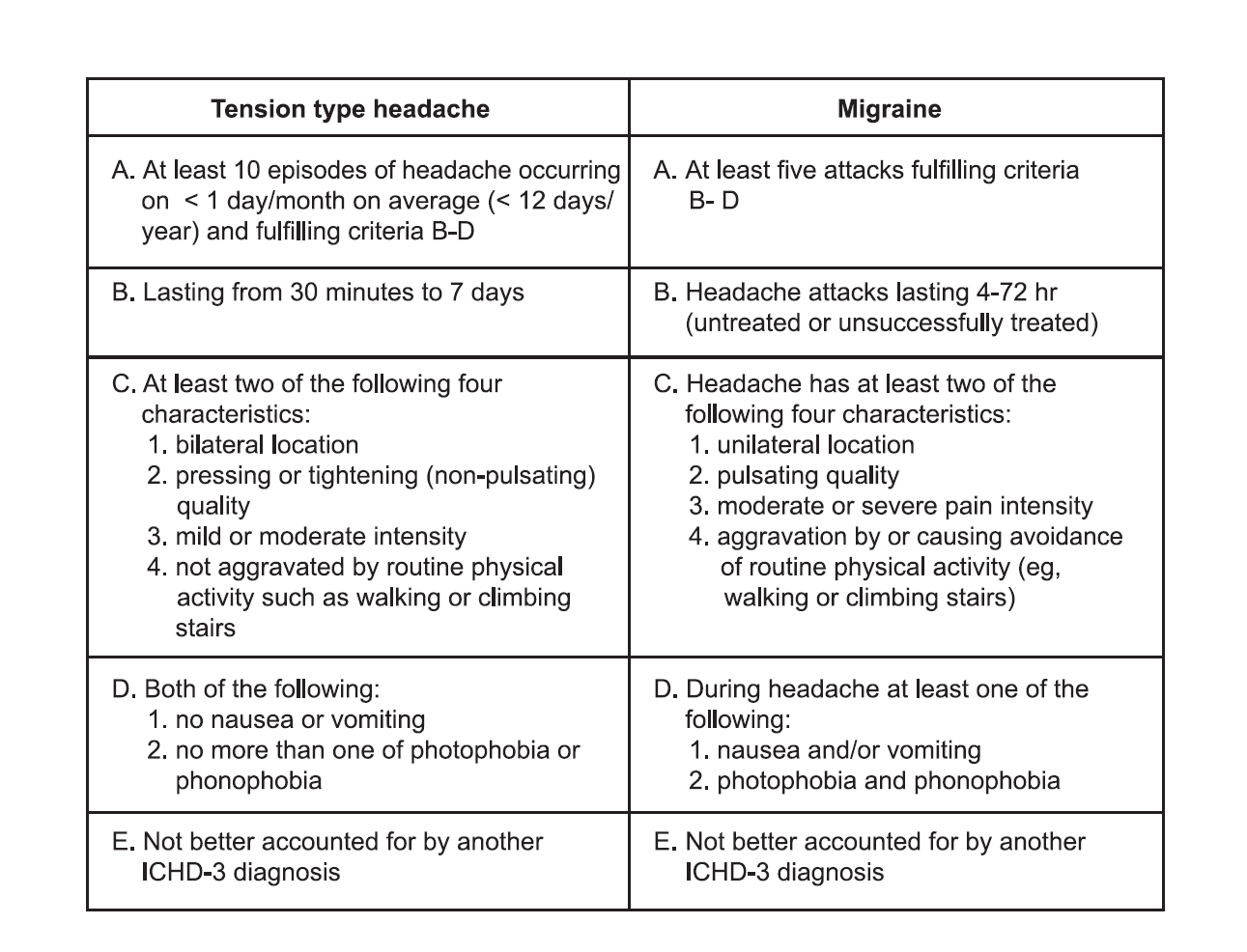
Occasionally, migraine could present in a bilateral location or with a mild pain degree. On the other hand, tension headaches could present unilaterally or with a moderate-to-severe pain degree that makes it more challenging to give the correct diagnosis. But the important clinical feature that is not present in tension headaches is nausea and/or vomiting, as IHS criteria are valuable in decreasing missed diagnoses1
In the Landmark and Spectrum studies, a review of patients' headache diaries revealed that more than 30% of patients initially diagnosed with tension-type or episodic headaches, met the IHS criteria for migraine headache2-3
Apart from misdiagnosis as tension-type headache, migraine may also be misdiagnosed as sinus headache, an eye strain headache, or a headache from high blood pressure.
Occasionally, migraine could present in a bilateral location or with a mild pain degree. On the other hand, tension headaches could present unilaterally or with a moderate-to-severe pain degree that makes it more challenging to give the correct diagnosis. But the important clinical feature that is not present in tension headaches is nausea and/or vomiting, as IHS criteria are valuable in decreasing missed diagnoses1
In the Landmark and Spectrum studies, a review of patients' headache diaries revealed that more than 30% of patients initially diagnosed with tension-type or episodic headaches, met the IHS criteria for migraine headache2-3
Apart from misdiagnosis as tension-type headache, migraine may also be misdiagnosed as sinus headache, an eye strain headache, or a headache from high blood pressure.




