A 55-year old right-handed woman, previously healthy, was referred from Ophthalmology service for evaluation of visual changes and progressive symptoms of cognitive decline over the past four years. She had fourteen years of formal education and a degree in Management and previously taught Chinese language. There was no history of head trauma, infection, psychiatric disease, or illicit drug use and no family history of neurodegenerative diseases. She initially reported difficulty reading and writing. She wrote sentences with missing words and could not write in one line. Most striking was her inability to locate things that were directly in front of her. Although she was able to name objects when presented individually, focusing on multiple objects on a screen was a challenge. Over the next two years, she had difficulty with simple arithmetic. She wore clothes inside out, wore a shoe on one foot and a slipper on the other. She was lost in places previously familiar to her and would follow unfamiliar individuals in a crowd. She confused items, rooms and faces, eventually needing assistance in choosing clothes for dressing, meal preparation, using the telephone, traveling, handling finances and taking medications.
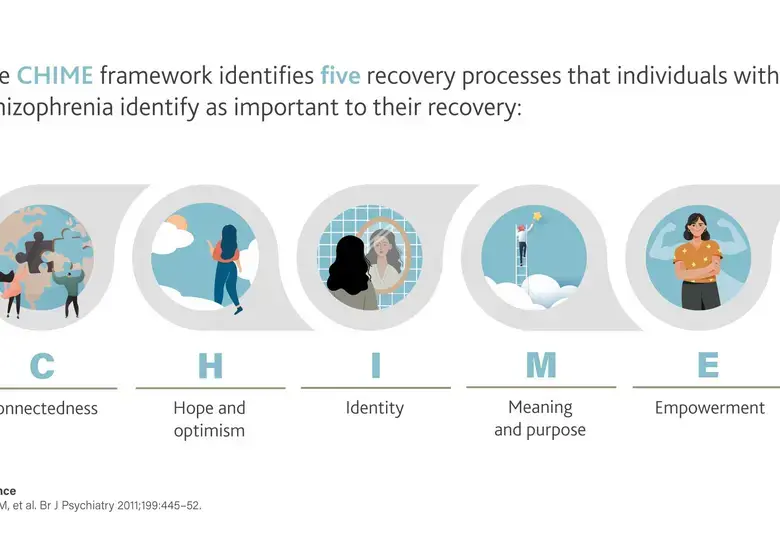
Clock drawing test was unsatisfactory with missing numbers (Fig. 1). Neuropsychological evaluation revealed moderate to severe cognitive impairment in all explored domains. All visual tasks were severely impaired, particularly attempts to integrate a complex visual picture into a meaningful whole. She had difficulty reaching for a stationary object held in front of her. A strong tendency to fix gaze on a single object was noted. Laboratory tests were negative for thyroid disease, metabolic disorders, and inflammatory or autoimmune diseases. Cranial MRI showed predominant parieto-occipital atrophy, more evident in the left hemisphere. FDG-PET showed marked posterior hypometabolism bilaterally (Fig 2).
Fig 1. Clock drawing test in 2014 (left), 2017 (middle) and 2018 (right) highlight progressive deficits in constructional ability.
Fig 2. Fluoro-deoxyglucose PET images. Generalized decreased FDG uptake in the biparietal, bitemporal and bi- occipital lobes with mild decreased uptake in the bifrontal lobes.
WHAT IS POSTERIOR CORTICAL ATROPHY?
Posterior Cortical Atrophy (PCA) is a progressive dementia with a young onset (late 50s and early 60s1) presenting with visuospatial and visuoperceptual challenges. One of the most frequent visual manifestations in PCA is simultanagnosia (above 90%)2 wherein the individual is unable to synthesize the overall meaning of the visual scene despite being able to recognize single elements. Perceptual organization and processing speed present as a bigger challenge compared to verbal comprehension and working memory due to visual disorientation (failure to track), ocular apraxia (failure to generate saccades), reverse-size phenomenon (difficulty reading large texts) and optic ataxia (inability to reach for objects under visual guidance)1. Cranial MRI and PET scans show bilateral parieto-occipital atrophy and hypometabolism.
Alzheimer’s Disease is the most common underlying disease pathology and as the disease progresses, PCA ultimately leads to a more diffuse pattern of cognitive dysfunction. Patients present with simultanagnosia and spatial disorientation, which are often missed by routine ophthalmologic and neurologic exams, causing delay in diagnosis. The clinical features of reported cases are heterogenous, leading to a classification of different variants and underlying pathologies. Due to the presenile onset of disease and variability of clinical features as the initial presentation, recognition of these symptoms is crucial to avoid misdiagnosis.