When a room full of attendees of the recent European Congress of Psychiatry held in Paris were asked “Do we need to abandon the current schizophrenia construct?” the response was inconclusive – with seemingly half in favour and half against.1 Such is the nature of this hotly debated topic, with multiple considerations to be assessed there is no one definitive answer. However, due to the far-reaching implications for schizophrenia diagnosis, treatment and outcomes, it is nevertheless an important debate to have.
The current schizophrenia construct
Since psychiatrist Eugen Bleuler first coined the term schizophrenia, there have been many subsequent attempts to define it. Recently, descriptions have come from the latest editions of the World Health Organization (WHO)’s International Classification of Diseases (ICD) and the American Psychiatric Association (APA)’s Diagnostic and Statistical Manual of Mental Disorder (DSM).2
However, Bleuler never intended for schizophrenia to be a singular term. “Groups of schizophrenias” was instead meant as an umbrella term for several psychoses.2 The fact that the current ICD and DSM definitions have not moved away from “schizophrenia” to even something as simple as “schizophrenias” is the main source of contention. Detractors say it doesn’t do enough to recognize the heterogeneity of the disorder. There have been many attempts to address this by identifying different subtypes, however this still pushes the notion that within schizophrenia exists a core pathognomonic symptom that links them all together, an idea that may not have a clinical basis.2
“Groups of schizophrenias” was meant as an umbrella term for several psychoses
The challenges finding a unifying core symptom in schizophrenia
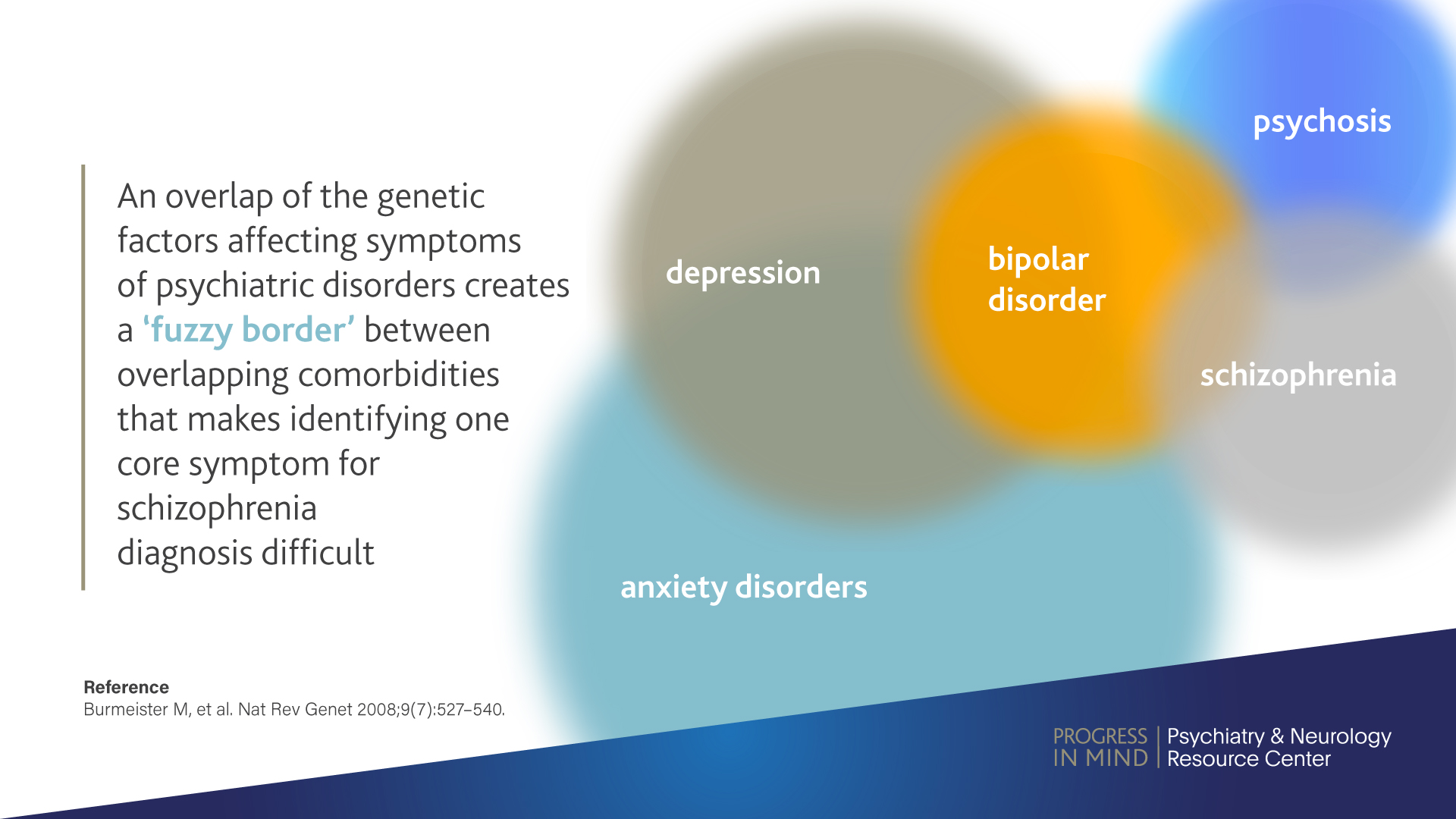
The emotional, social and executive functions of the brain require precisely choreographed patterns of interaction between bio-behavioural modules of the brain, with the clinical phenotype of diseases, such as schizophrenia characterized by their dysfunction.3 There exists an overlap of the genetic factors affecting symptoms of psychiatric disorders. This creates a ‘fuzzy border’ between overlapping comorbidities that makes identifying one core symptom for schizophrenia diagnosis difficult.4
1152-lun-sp1-epa-article-3-infographic-web-c.jpg
All this means that there is widespread uncertainty about the diagnostic accuracy of first rank symptoms (FRS) for diagnosing schizophrenia. Symptoms that include:5
- Auditory and/or somatic hallucinations
- Thought withdrawal, insertion and interruption
- Thought broadcasting
- Delusional perception
- Feelings or actions as made or influenced by external agent
First rank symptoms can be found in 29% of patients with affective disorders, are often unstable, and are poor predictors of outcomes2
In both DSM-IV and ICD-10, FRS were given priority in the diagnostic criteria even though they are not specific to schizophrenia. Studies have shown that FRS can be found in 29% of patients with affective disorders, are often unstable, and are poor predictors of outcomes.2
Stigma and misunderstanding surrounding schizophrenia
Another consideration for abandoning the current construct is that the term schizophrenia is unfortunately associated to a high level of stigma, acquiring a derogatory connotation over its long history. It has often been interpreted as “split personality”, thus mixing up schizophrenia and dissociative identity disorder and adding a level of misunderstanding to an already complex disorder. Patients and caregivers often complain about a scarcity of sensitivity, even from clinicians, so a change to terminology may help address this.2
The importance of the current schizophrenia construct
However, it is undeniable that the attempts made to define schizophrenia, as imperfect as they may be, have had a positive impact on treatment. The current diagnostic criteria have improved reliability in formulating the diagnosis across health systems, particularly in those utilizing structured interviews. These criteria provide evidence that can be used to establish diagnosis and treatment guidelines, and to provide information on patient outcomes. Additionally, they have made communication among clinicians, patients and families less ambiguous, and can also be used for education and training purposes.2
Updating and reinventing the current schizophrenia construct
According to Silvana Galderisi, Professor of Psychiatry at the University of Campania Luigi Vanvitelli, we are not ready to abandon the current schizophrenia construct. Instead, Wolfgang Gaebel, Professor of Psychiatry at the University of Dusseldorf and chair of the ICD-11 working group on psychotic disorders, suggests it is time to update the construct.
This process has begun, with neither DSM-5 nor the ICD-11 assigning diagnostic priority to FRS. ICD-11 has been modified further, with the introduction of cognitive symptoms as symptoms of schizophrenia “due to compelling evidence, they are closely related to clinically relevant functional impairments”.
Moving forward, the Research Domain Criteria (RDoC) project believes that although useful, the current definitions are insufficient to fully capture the biological and pathophysiological nature of the patient’s condition.6 RDoC aims to provide an effective bridge between behavior and the brain by providing a potential framework for quantitatively evaluating functional data for clinical prediction and/or biological research.6
Looking to the future
We are not ready to abandon the current schizophrenia construct, but should be prepared to do so – Silvana Galderisi
Additionally, either now or in the near future, new digital health technologies may be utilized to collect the additional data needed for comprehensive schizophrenia treatment. Smart phone-based surveys or wearable sensors could provide a deeper insight into each patient’s condition, whilst artificial intelligence (AI) and machine learning may one day be involved in precision psychiatry.7,8
It will be hard to implement the change needed whilst there is still so much disagreement among clinicians as to whether the current schizophrenia construct is failing in the first place. It seems that Professor Galderisi may be right in that: “we are not ready to abandon the current schizophrenia construct, but should be prepared to do so.”