The COVID-19 pandemic represents a ‘triple threat’, impacting not only the physical health of citizens worldwide, but also their economic status, and mental health and wellbeing.
The prevalence of major depressive disorder and depressive symptoms has increased worldwide over the past year,1,2 triggering what some are referring to as a mental health tsunami.3 Beyond exacerbating symptoms in patients with pre-existing mental health conditions, the pandemic has increased the prevalence of new cases of major depressive disorder and depressive symptoms in the general population, and in COVID-19 survivors.1,4,5
Experience from past viral outbreaks, including severe acute respiratory syndrome and Middle East respiratory syndrome, indicate that the psychopathological consequences of COVID-19 will likely be long lasting and require careful monitoring.6–8
Effect of COVID-19 on patients with MDD
The COVID-19 pandemic can be considered a global traumatic event from a mental health perspective, owing to its psychological burden and associated stressors, including the unpredictable nature of the disease, economic uncertainty, lockdown measures, and social isolation.1,9,10 A ~three-fold higher prevalence of depressive symptoms/major depressive disorder (MDD) has been observed compared to before the COVID-19 pandemic.1,5
The COVID-19 pandemic constitutes a traumatic event
Psychiatric patients, including those with MDD, are particularly vulnerable to the impact of the COVID-19 pandemic for a number of reasons.11
Firstly, they may experience relapses in their mental health condition triggered by factors such as social isolation, fear of infection, and economic uncertainty.12,13 Many patients have also struggled with the disruption to their daily routine and grieve their pre-pandemic lives. They may also be at a heightened risk of contracting the virus itself, due to behavioural and socioeconomic factors, as well as elevated levels of inflammation.14
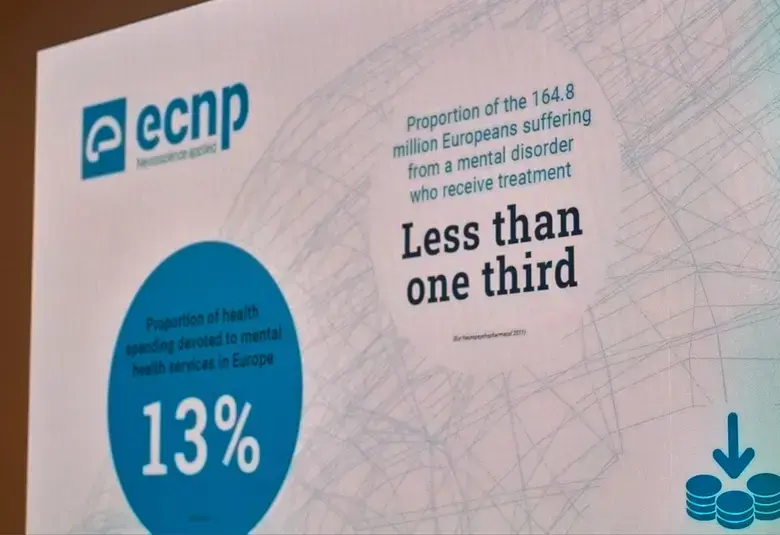
Reduced access to mental health services has posed an additional challenge for psychiatric patients,15 with many clinicians feeling that the impact of the pandemic on patient care has been largely negative. Telemedicine has, however, provided some benefits in psychiatry, including increased privacy and fewer missed appointments.16
Patients with MDD face additional challenges during the COVID-19 pandemic
Impact and possible mechanisms of long COVID
‘Long COVID’, or ‘post-COVID-19 syndrome’ has been observed in a subset of the population and is defined by the UK National Institute for Health and Care Excellence (NICE) as “signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis.”17
The clinical features of long COVID include chronic cognitive deficits, depression, sleep difficulties, persistent fatigue, and anhedonia.17,18 Survivors have described a feeling of ‘brain fog’, which may encompass all, or a combination of these features.19 Cognitive dysfunction resulting from long COVID will likely have a significant impact on survivors’ ability to return to everyday functioning.20 Parallels have therefore been made between long COVID and MDD, given the overlap in core symptomology and physical, emotional, and cognitive burdens.
Parallels observed between long COVID and symptoms of MDD
It is hypothesised that the symptoms of long COVID may be driven by an elevated immune response. Both COVID-19 and depression have been associated with high plasma levels of inflammatory mediators,21–23 and the therapeutic efficacy of antidepressants in MDD may be partly attributed to their anti-inflammatory properties.24 An observational study of patients hospitalised for COVID-19 suggested a lower risk of intubation or death in those treated with antidepressants compared to those without.25
Mental health and MDD in the COVID-19 era and beyond
More resilient individuals, for example those with more established support networks or with a stronger sense of spirituality, are less likely to experience symptoms of depression or anxiety as a result of the pandemic.26 The 2021 World Happiness Report, published by the United Nations Sustainable Development Solutions Network, revealed commonalities such as social connectedness and daily physical activity between the happiest groups.27
Overall, the COVID-19 pandemic has created a substantial burden on global mental health.1,2,5 Anhedonia has been shown to be a predictor of severe depression during the pandemic, and patients with MDD have experienced exacerbations in symptoms such as fatigue and poor sleep.28–30 Reports of these symptoms, in addition to cognitive impairment, have also been elevated in COVID-19 survivors.4,18,31–33 In order to best support patients with MDD, a treatment option should therefore be considered that both ameliorates the symptoms of MDD and promotes subsequent functional recovery.34
This article was developed in follow-up to a promotional webinar discussing COVID-19 and vortioxetine (Brintellix®).
Educational and financial support provided by Lundbeck.
For the latest updates on sea.progress.im, subscribe to our Telegram Channel https://bit.ly/telePiM
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.