The advent of COVID-19 vaccines has raised questions on whether vaccines impact on the management of migraine and other headache disorders. Speaking at #AHSAM21, Dr Amy Gelfand, UCSF Weill Institute for Neurosciences sought to answer some of these questions based on current evidence for any interactions between vaccines and migraine treatments and potential risks of vaccinations. There is a risk of rare serious adverse events with COVID-19 vaccines and the differentiation of migraine from other serious causes of headache with clotting events occurring after vaccination is an important distinction to make in women aged 18–49 years.
Questions around CGRP antibodies and vaccines
Clinical questions fall roughly into two broad categories:
There are no data to suggest that CGRP antibodies in any way interfere with COVID-19 vaccine immunogenicity, safety, or efficacy
- Does migraine treatment impair the efficacy or impact the safety of the COVID-19 vaccine? and
- Does the COVID-19 vaccine adversely impact the efficacy of migraine treatments?
With regard to CGRP antibodies, there is no immunological or clinical reason to think that these would impair the body’s immunological response to any vaccine.1 While there are CGRP receptors on lymphocytes, macrophages, and mast cells, and CGRP may have a role in pro- and anti-inflammatory actions, there is no evidence from clinical trials that CGRP antibodies are immunosuppressive or myelosuppressive. The nature of CGRP antibodies is that they have very narrow specificity limited to their defined target.1
On the other side of the coin, there is no reason to think that antibodies to the spike protein of the SARS-CoV-2 virus induced by COVID-19 vaccines would neutralize antibodies to CGRP or its receptor and make the CGRP antibody migraine preventives less effective.1 Consequently, Dr Gelfand said there is no apparent rationale to retime CGRP antibody treatment.
There is no evidence that CGRP antibody preventive treatment needs to be delayed or retimed around timing of COVID-19 vaccination
Differentiating migraine from CVST with thrombocytopenia
Adenovirus vector vaccines for COVID-19 have been associated with rare cases of cerebral venous sinus thrombosis (CVST) with thrombocytopenia, and thrombosis in other major vessels – thrombosis thrombocytopenia syndrome (TTS). The proposed mechanism is akin to autoimmune heparin-induced thrombocytopenia (HIT), in that platelet-activating antibodies develop.2,3
The epidemiology of TTS overlaps with migraine epidemiology. TTS risk is predominantly among women aged 18-49 years (7.0 TTS cases/million), and highest among those aged 30-39 years (11.8 TTS cases/million).4
This has raised the question of how healthcare professionals can differentiate between migraine and CVST with thrombocytopenia among patients with migraine who develop a headache after receiving an adenovirus-vector COVID-19 vaccine administration.
In our patients, how do we tell if a headache that develops after an adenovirus-vector COVID-19 vaccination is migraine versus CVST?
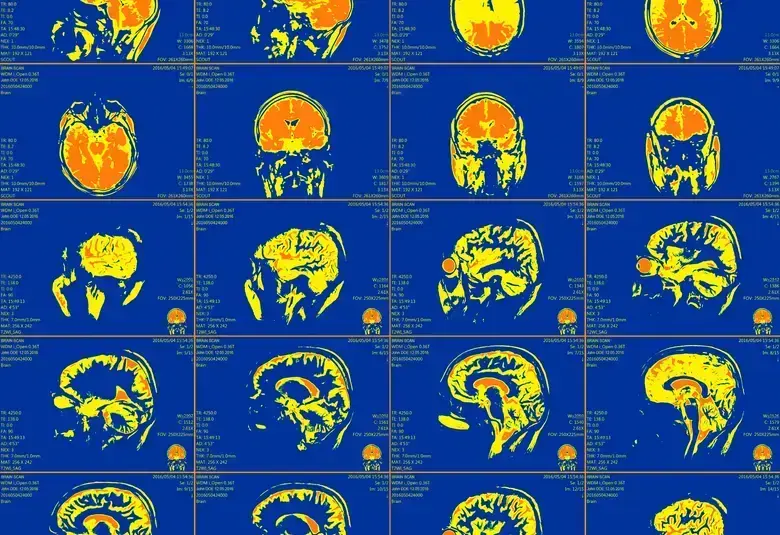
Dr Gelfand suggested that clinical clues that may be used to differentiate between migraine headache and CVST include the timing of onset (headache beginning 6-15 days after vaccination), epidemiology, and detection of any unusual headache features or symptoms of clot in other parts of the body.5 In uncertain cases, platelet count testing and MRI/MRV imaging of the brain may be necessary; however, the risk of CVST is still very low.
For the latest updates on sea.progress.im, subscribe to our Telegram Channel https://bit.ly/telePiM
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.