How might meningeal immune cells influence neural activity and lead to the symptoms of migraine? asked Professor Andrew Russo, University of Iowa, IA, at the Virtual Scottsdale Headache Symposium 2020.
How might meningeal immune cells influence neural activity and lead to the symptoms of migraine? asked Professor Andrew Russo, University of Iowa, IA, at the Virtual Scottsdale Headache Symposium 2020.
The meningeal immune cells
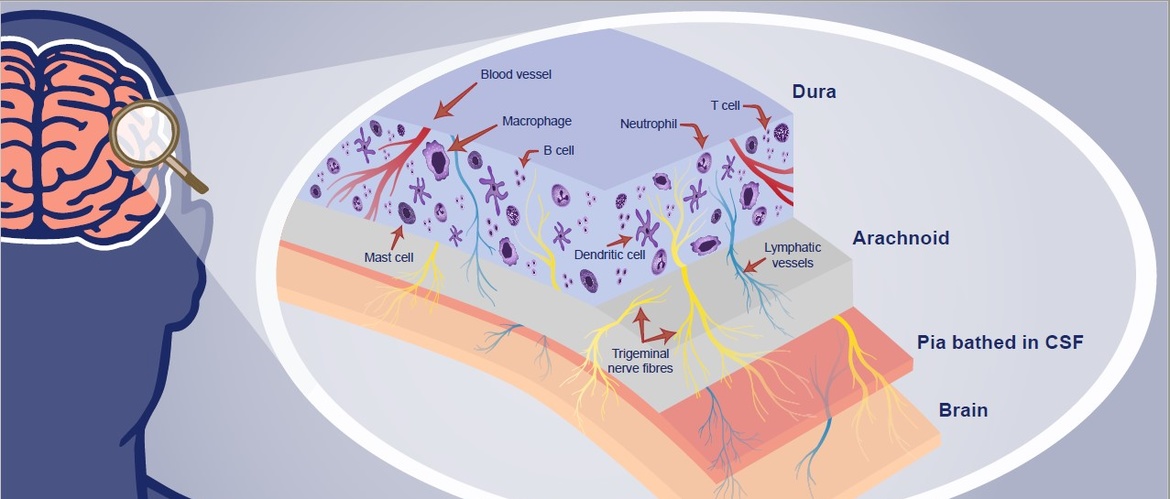
The three layers of the meninges do not provide equal access to the brain
The dural layer of the meninges contains many types of innate and adaptive immune cells, including macrophages, dendritic cells, mast cells, innate lymphoid cells, neutrophils, and B and T cells,1,2 said Professor Russo.
Dura lies adjacent to the skull and also contains trigeminal nerve fibers, lymphatic vessels, and fenestrated blood vessels.1,2
Pia lies within the BBB
Professor Russo highlighted that the three layers of the meninges are not equal in terms of accessibility to the brain.
Arachnoid lies contiguous to the dura and is the avascular impermeable barrier between brain CSF in the subarachnoid space and extracellular fluid. Molecules cannot diffuse freely from the dura mater into the subarachnoid space.1,2
Pia lies beneath the arachnoid, is within the blood–brain barrier (BBB), and is bathed in cerebrospinal fluid (CSF).1,2
Trigeminal nerve fibres straddle the meningeal BBB
Trigeminal nerve can be activated from within and outside the BBB
Trigeminal nerve fibers are not only present in the dura, but collateral branches descend into the pia—so straddle the BBB,2 said Professor Russo. As a result:
- trigeminal fibers in the dura are outside the BBB
- trigeminal fibers in the pia are inside the BBB
The trigeminal nerve can therefore be activated from within and outside the BBB and can communicate with the brain across the meninges.2
Two-way communication between neurons and immune cells
Neuronal factors released from nociceptor sensory neurons drive the immune response
Meningeal lymphatic and CNS glymphatic systems transport signalling molecules within the brain and to the meninges.3 This enables two-way communication between neurons in brain parenchyma and immune cells in the meninges, commented Professor Russo:
- immune cells can “talk to” and activate neurons leading to peripheral sensitization4
- activated afferent sensory nerves can “talk to” immune cells through the release of neuropeptides, which drive inflammation4
Professor Russo concluded that more research is now needed to understand the actions of neuropeptides such as calcitonin gene-related peptide (CGRP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the meninges, periphery, brain, and immune cells.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.